A 21 year old female patient with fever, vomiting and generalised body pains
Hi, I am G Sai Karthik, 3rd Sem Medical Student. This is an online e-log book to discuss our patient's health data shared after taking his/her/guardian's consent . This also reflects patient centered care and online learning portfolio.
- This E-log book also reflects my patient-centered online learning portfolio and of course, your valuable inputs and feedbacks are most welcome through the comments box provided at the very end. HAPPY READING.
- * This is an ongoing case. I am in the process of updating and editing this ELOG as and when required
CHIEF COMPLAINT:
A 21 year old female patient who is a student came to the casualty on 22nd of July with complaints of high fever, vomitings and generalised body pains.
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 8 days ago. Then she developed high fever on morning of 21st July associated with chills and generalised body aches.Later that evening she started vomiting (non-bilious) with food as content which was associated with abdominal pain.She had 6 episodes of vomiting that evening.Then she presented to the casualty on 22nd of July where she was examined and admitted for further treatment.
HISTORY OF PAST ILLNESS:
No history of similar complaints in the past.
Not a K/C/O HTN/T2DM/ASTHMA/CAD/CVA/EPILEPSY/TYPHOID.
The patient has history of frequent headaches.
PERSONAL HISTORY:
DIET:Mixed
APETTITE:Lost
BOWEL AND BLADDER:Regular
SLEEP:Normal/Adequate
AlLERGIC HISTORY: Allergic to Brinjal, Roselle leaves and Potato
The patient has no history alcohol consumption, smoking of cigarettes and chewing of beetle nuts.
FAMILY HISTORY:
No significant family history.
GENERAL EXAMINATION:
The patient is moderately build and moderately nourished.
No pallor/No cyanosis/No clubbing of fingers/No lymphadenopathy/No icterus/No Oedema of feet
VITALS:
TEMPERATURE:Febrile(100 degree Fahrenheit)
PULSE RATE:88 bpm
BLOOD PRESSURE:110/70 mm Hg
SpO2:98%
GRBS:101mg/dL
SYSTEMIC EXAMINATION:
CVS:S1 S2 Heard,no murmurs
R/s:BAE+,Clear
CNS:Higher motor functions intact
P/A:Soft,Non tender,BS+
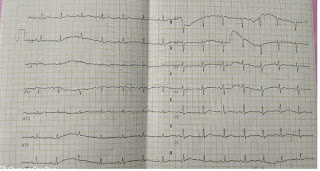
INVESTIGATIONS:
INVESTIGATION CHART
The investigation chart shows a reduction of platelet count.
USG ABDOMEN
FOLLOW UP: On the evening of 27th of July, the platelet count of the patient went up from 36000 to 46000 cells per microlitre. There were no episodes of high fever since then.












Comments
Post a Comment